November 11, 2020
Overview
Throughout the novel coronavirus (COVID-19) pandemic, healthcare providers have fought a war on two fronts: protect vulnerable patients and prevent the hospital system from being overrun with COVID-19 cases.
This has meant patients and practitioners have been forced into a socially distant relationship — all of which has led to the dramatic acceleration in the development of virtual solutions.
Even before the pandemic, telemedicine use was rising, according to an American Medical Association (AMA) survey of physicians: from 14 percent of respondents in 2016 to 28 percent in 2019. With the onset of the COVID-19 pandemic, an estimated 60 percent to 90 percent of U.S. physicians are using some form of virtual care services today, according to the AMA, half of them likely for the first time.
Post-pandemic, both patients and providers will continue to seek virtual care options, many of them through models that integrate virtual care with in-person healthcare services. Such an integrated approach could allow more personalized care, improve patient access and reduce employer costs significantly — up to 15 percent, according to Aon estimates.
“When the pandemic hit, one of the things many health systems did almost overnight was create a telemedicine program,” says Dave Guilmette, president of Global Health Solutions at Aon. “Now a lot of them are looking at ways to maintain those programs. They’re looking at telemedicine and other virtual care options as a pathway to provide new and enhanced services to healthcare consumers.”
In Depth
Telehealth adoption has risen sharply since the start of the pandemic: McKinsey found that as of late April 2020, 46 percent of U.S. consumers were using telehealth to replace cancelled healthcare visits compared to 11 percent in 2019. With both healthcare consumers and providers moving rapidly to embrace telehealth, virtual healthcare could represent $250 billion of U.S. healthcare spending, according to McKinsey.
It’s not just a U.S. phenomenon. “In the U.K. there’s a big government focus on digital health,” says Dr. Avneet Kaur, principal consultant, Health Solutions EMEA at Aon. “The public health landscape is moving towards mainstreaming digital health over the next 5 to 7 years. The European Centre for Disease Prevention and Control is giving a very good boost to digital health — they’re making sure that health consultations are becoming borderless. Germany’s digital health act, introduced this year, will get insurers to cover costs of doctor-prescribed apps.”
Some things can’t be done virtually — administering a vaccine, drawing blood for lab work. And in many cases, virtual care will supplement, rather than replace, in-person doctor visits. “For many chronic conditions, face-to-face visits must occur at some point for quality of care — but telehealth can help reduce a number of on-site appointments throughout the year,” says Wendy Smith, senior vice president and national leader of Delivery System Transformation at Aon.
But that still leaves a wide range of opportunity for virtual care — during COVID-19 and beyond.
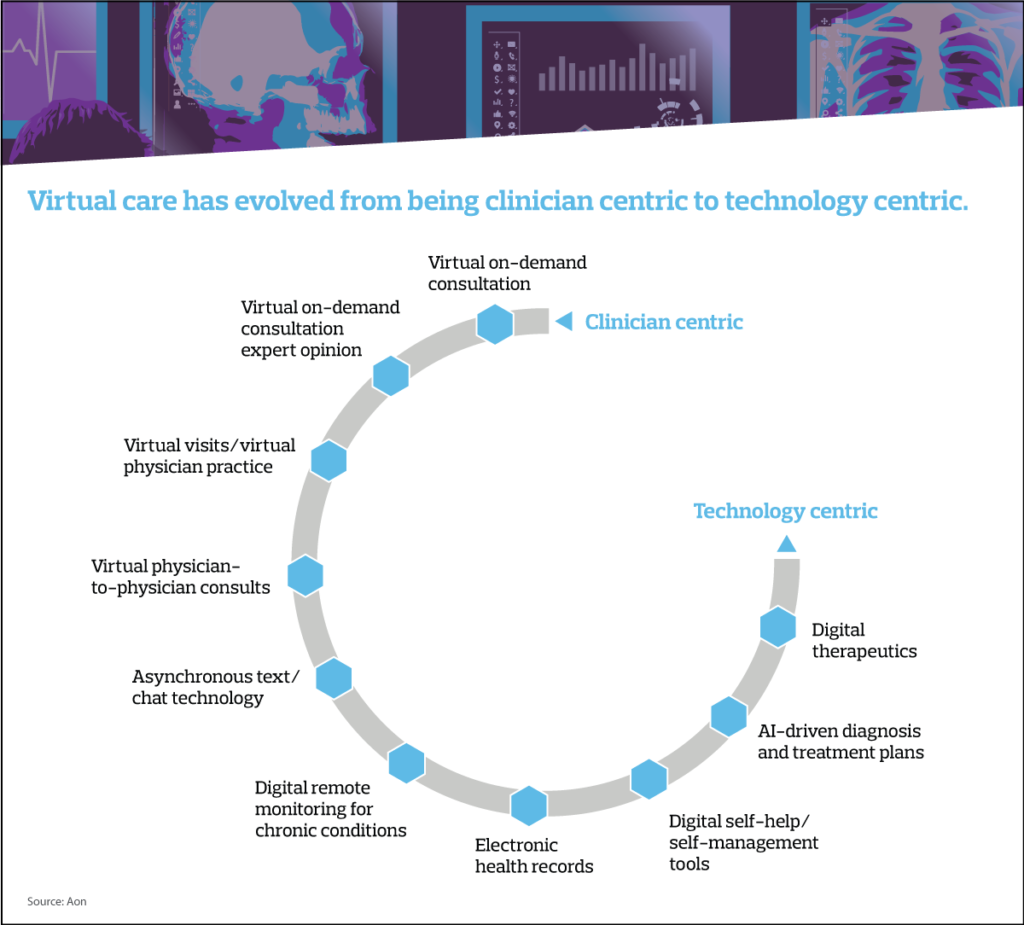
Moving from expert – to tech-centric care
Virtual care originally showed up in healthcare as on-demand consultation with a health professional for urgent, one-time physical needs, and ongoing care, such as for mental health. The model has already evolved. The core focus of virtual care is expanding from doctors and medical specialists to technology that can assist, or even replace, healthcare professionals.
In a market where 26 percent of U.S. adults — and even more millennials — do not have a relationship with a primary care physician, virtual care can fill the gap. “Everyone can benefit from a ‘health home’ — a primary healthcare professional who understands the person and can coordinate care across the spectrum of healthcare needs,” says Janet Faircloth, senior vice president and national leader of virtual care strategy at Aon. “Virtual care offers convenient 24/7 access to primary care and leverages technology to expand the capacity of primary care physicians.”
In Asia, artificial intelligence (AI) expands physicians’ capacity by prescreening and diagnosing patients. AI-driven self-management tools are available for many chronic conditions. Meanwhile, tools for asynchronous texting — messaging over a period of time rather than in the moment — are allowing physicians to review data, then make and share diagnosis and treatment recommendations with patients without a real-time conversation.
“In a region where, for a long time, trusting a doctor meant knowing them through their reputation or seeing it for yourself, the virtual model of care offers a new perspective on what is possible with mutual trust between provider and user,” says Dr. Amitabh Deka, head of wellbeing solutions, South Asia and Aon Care.
“Technology is the third element of the trust triangle. Both doctors and patients continue to be measured in their dependency on technology for safeguarding their interests. Citizens have leveraged technology much more in recent years for other services — but the data sensitivity involved for healthcare is of a different nature altogether.”
Virtual care is also growing in importance in Latin America. “Pandemic-driven regulatory changes and social distancing measures enabled an increase in employers seeking telehealth options and motivated patients to try telehealth for the first time,” says Violetta Ostafin, CEO of Health Solutions, Aon Latin America. In a recent Aon survey, over 37 percent of employers in the region reported introducing a telemedicine option during the pandemic.
In Latin America, providers are adapting virtual care formats to familiar and available in-market options, Ostafin says. For example, mobile messaging may be used, and where broadband and high-quality video connectivity may not be available, text-based services can provide access and support virtual consultations.
“Virtual care has the potential to become a more patient-centric, accessible and cost-effective healthcare system,” says Guilmette. “But to tap its full potential, the ecosystem has to evolve with it.”
To build this new ecosystem, progress will have to be made in areas such as healthcare insurers and providers agreeing upon refreshed reimbursement formulas, and employers deciding how to integrate virtual care into their health plan offerings.
Five keys to employer virtual care strategy
For employers, introducing virtual care for health plan participants means developing a solid strategy. Consider these five key steps along the way:
1. Know your people and plan around their needs. “Analyzing usage trends and costs for various types of care — urgent, primary, specialized, continuous — can help employers determine how virtual care can reduce healthcare costs and improve employee health outcomes,” says Ostafin.
Employers can gain insights through data and analytics into employees’ health risks, disparities and conditions. Where are there potential gaps in access and support?
2. Define success clearly. “What outcomes and key metrics do you want your virtual care plan to meet, and by when?” asks Kaur. “The more expansive the desired outcomes, the more extensive the virtual care strategy should be.”
3. Create an experience that improves engagement. Adding the option of virtual care can increase employees’ confusion with an already complex healthcare system. “The goal is to create a plan that connects employees and their families with the right resources at the right time, provides necessary information and integrates seamlessly with the rest of the healthcare program,” says Deka.
Foster employee engagement by streamlining the points of entry to care. A few ideas: a virtual primary care platform, a concierge navigation system or a digital platform that employees are already using.
4. Select partners that share your vision. Establish the criteria for selecting the vendors and healthcare providers that will make the virtual care strategy a reality: How intuitive is the technology? What is their clinical approach? What experience and credentials do their medical practitioners have? How would they handle expansion as demand grows?
5. Establish targets and accountability. All partners in the virtual care strategy should be held accountable for its success, regardless of their role, says Guilmette.
“Use performance guarantees and service-level agreements that are directly tied to integration, coordination and overall results to motivate stakeholders and keep them aligned. Adopt a methodology to measure your strategy’s success and ask your partners to agree to it,” Guilmette says.
Telehealth and expanding access to care
With the promise of improving both the quality of care and access to it, along with reducing healthcare costs, telehealth holds a role in healthcare plans of the future.
“There are many gaps in healthcare that have to be closed,” says Smith. “For many conditions, integrating telehealth with face-to-face visits, when appropriate, is a way to close those gaps, improve the quality of healthcare delivery and reduce healthcare costs.”
This document has been provided as an informational resource for Aon clients and business partners. It is intended to provide general guidance on potential exposures and is not intended to provide medical advice or address medical concerns or specific risk circumstances. Information given in this document is of a general nature, and Aon cannot be held liable for the guidance provided. We strongly encourage readers to seek additional safety, medical and epidemiological information from credible sources such as the World Health Organization. As regards insurance coverage questions, whether coverage applies or a policy will respond to any risk or circumstance is subject to the specific terms and conditions of the insurance policies and contracts at issue and the relevant underwriter determinations.
While care has been taken in the production of this document, and the information contained within it has been obtained from sources that Aon believes to be reliable, Aon does not warrant, represent or guarantee the accuracy, adequacy, completeness or fitness for any purpose of the report or any part of it and can accept no liability for any loss incurred in any way by any person who may rely on it. Any recipient shall be responsible for the use to which it puts this document. This document has been compiled using information available to us up to its date of publication.
The post Telehealth’s Rise: 5 Keys To A Virtual Care Strategy appeared first on The One Brief.